Presented by: Tom L. Rosamond, MD, MSc, FAHA, FACC, FASE
Dr. Thomas Rosamond is Board Certified in Cardiovascular Disease. Dr. Rosamond is the Division Chief of Cardiovascular Imaging and Medical Director of Non-Invasive Imaging Services at The University of Kansas Health System. He earned his Postdoctoral Fellowship in Cardiovascular Magnetic Resonance Imaging at Washington University School of Medicine -Barnes Jewish Hospital in St. Louis, Missouri.
Precision Cardiology: Navigating Complex Coronary Artery Challenges
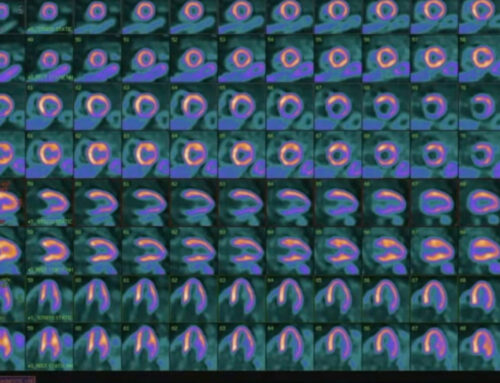
The landscape of cardiovascular diagnostics is becoming increasingly sophisticated, especially when it comes to understanding the complexities of coronary artery disease (CAD). Traditional imaging techniques, while invaluable, often fail to provide a complete picture of coronary blood flow and its dynamics, leaving clinicians with critical gaps in information. Modern advancements in diagnostic strategies are reshaping our ability to assess coronary flow in unprecedented detail, enabling more precise decision-making and personalized interventions. This article explores the nuanced nature of coronary flow dynamics, key diagnostic insights, and the evolving role of precision cardiology in guiding effective treatment strategies.
The Nuanced Landscape of Coronary Flow Dynamics
In the past, coronary artery diagnostics have predominantly focused on detecting significant blockages or stenosis in the epicardial arteries. However, this approach often overlooks the subtle, yet clinically important, dynamics of coronary flow. The modern paradigm of precision cardiology demands a deeper understanding of coronary circulation, including the intricate patterns of blood flow through different vascular territories, and how these patterns relate to patient symptoms and clinical outcomes. In particular, coronary flow dynamics encompass not just the degree of stenosis but also how the heart’s blood supply responds to stress, how perfusion deficits manifest, and which regions of the heart are most affected.
Key Diagnostic Insights
Comprehensive Flow Assessment
A fundamental aspect of precision cardiology is the use of advanced diagnostic tools that provide a comprehensive, multi-faceted view of coronary blood flow. This allows clinicians to move beyond simply identifying blockages and delve into how these blockages, and other vascular challenges, impact overall heart function.
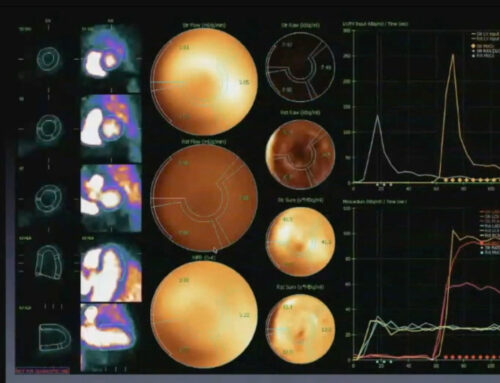
- Multi-Territorial Flow Evaluation: The ability to assess flow across multiple coronary territories—right coronary artery (RCA), left anterior descending artery (LAD), and left circumflex artery (LCx)—is crucial in determining the full extent of coronary involvement. Understanding how blood flows through each of these territories and identifying areas with compromised flow can direct the clinical focus to regions that require more urgent attention.
- Identifying Primary vs. Secondary Vascular Challenges: Not all areas of impaired flow are equally significant. In many cases, one territory will be the primary driver of ischemia, while others may be secondary or compensatory in nature. By accurately identifying which vascular territories are most affected, clinicians can make more targeted and effective intervention decisions.
- Precise Localization of Flow Limitations: Advanced imaging technologies, such as coronary flow reserve (CFR) assessments and fractional flow reserve (FFR) measurements, enable clinicians to precisely localize areas of flow limitation, even in the absence of significant coronary artery narrowing. This fine-level detail allows for better alignment of clinical decisions with the true underlying pathology.
Critical Diagnostic Findings
Flow Territory Analysis
When assessing coronary flow dynamics, clinicians must evaluate how different coronary arteries contribute to myocardial perfusion. This approach helps to identify which territories are most at risk and which may warrant immediate intervention.
- Right Coronary Artery (RCA): Typically, the right coronary artery is a major contributor to coronary perfusion in many individuals. However, it is also more prone to developing significant ischemia due to its involvement in larger vascular territories and its sensitivity to changes in blood flow. For many patients, the RCA becomes the primary focus in intervention planning, particularly in cases where its flow reserve is reduced.
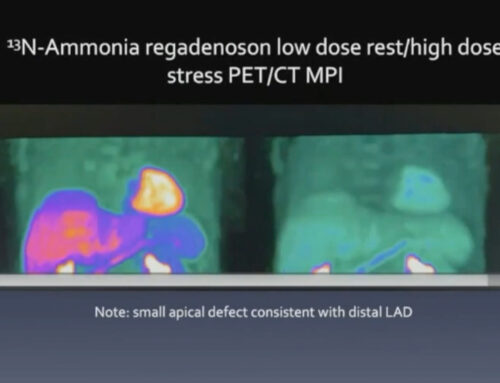
- Left Anterior Descending Artery (LAD): The LAD is often responsible for the majority of blood flow to the anterior wall of the left ventricle. In many cases, mild reductions in LAD flow may be present, especially in the early stages of coronary artery disease. These findings may not always warrant urgent intervention but should be closely monitored.
- Left Circumflex (LCx): The LCx tends to show secondary involvement in CAD, particularly when compensatory flow mechanisms have kicked in to offset deficiencies in the other coronary territories. Though less often a primary intervention target, recognizing LCx involvement can be critical in understanding the full scope of coronary impairment.
Advanced Diagnostic Strategies
Angiographic and Flow Data Integration
To optimize decision-making, angiographic findings must be integrated with flow reserve and other functional data. This combined approach provides a more complete picture of the coronary circulation, allowing clinicians to prioritize interventions more effectively.
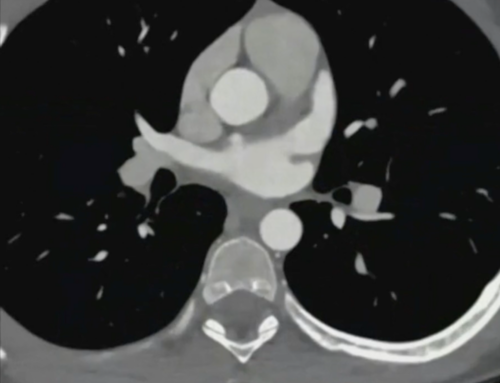
- Correlation Between Flow Data and Anatomical Findings: Traditional coronary angiography provides an excellent view of the anatomical features of coronary vessels, but it fails to show how well blood is actually flowing through those vessels. By correlating angiographic images with flow data, such as CFR or FFR, clinicians can assess the functional significance of any identified blockages and tailor their interventions accordingly.
- Identifying True Intervention Priorities: Not all blockages or narrowing in coronary arteries require revascularization. By incorporating flow data, clinicians can better identify which lesions are truly impairing perfusion and need intervention versus those that may be safely monitored without immediate treatment. This nuanced approach ensures that resources are allocated effectively and that patients are not subjected to unnecessary procedures.
- Understanding Complex Vascular Interactions: The coronary vasculature is a highly dynamic system, where changes in one area can affect flow in other regions. Advanced diagnostic tools help clinicians understand these complex interactions and their implications for patient management. For instance, compensatory mechanisms, such as the development of collateral circulation, may mask the need for intervention in some cases, while revealing it in others.
Intervention Decision-Making
Strategic Revascularization Approach
The goal of coronary intervention is not simply to open blocked arteries but to restore optimal perfusion across all coronary territories. To achieve this, a strategic approach based on comprehensive flow analysis is essential.
- Right Coronary Artery as Primary Focus: In many cases, the RCA will be the first area of focus due to its critical role in overall myocardial perfusion. When flow reserve is significantly diminished in the RCA, prompt revascularization can prevent further ischemic damage and improve long-term outcomes.
- Targeted Intervention Based on Comprehensive Flow Analysis: Using a combination of angiography, flow reserve measurements, and other diagnostic tools, clinicians can make informed decisions about which coronary lesions to treat first. This approach avoids unnecessary interventions and ensures that the most clinically relevant issues are addressed first.
- Avoiding Procedural Misallocation of Resources: By accurately assessing the functional significance of coronary lesions, clinicians can avoid over-treatment. For instance, a lesion that appears significant on angiography may not significantly impair myocardial perfusion and may not warrant immediate intervention. Conversely, a mild lesion may be functionally critical if it affects myocardial flow reserve. This targeted approach ensures better resource utilization and improves patient outcomes.
Normative Flow Data Considerations
Establishing Diagnostic Benchmarks
In order to interpret coronary flow data effectively, healthcare providers must rely on established benchmarks and normative ranges to determine whether observed values fall within the expected range.
- Stress and Rest Flow Measurements: A comprehensive assessment of coronary flow should include both stress and rest measurements. This provides insight into the coronary vasculature’s response to increased metabolic demand and helps identify early signs of ischemia that may not be evident at rest.
- Myocardial Flow Reserve (MFR) Quantification: Myocardial flow reserve is a key metric used to assess coronary flow capacity and its response to stress. Normal MFR values should be above 2.0, with values below this threshold suggesting a significant impairment of coronary flow. MFR quantification provides a reliable indicator of the functional status of the coronary arteries.
- Reference Ranges for Low-Likelihood Ischemic Patients: For patients with low likelihood of ischemia or coronary disease, establishing reference ranges for flow measurements helps to differentiate between normal variability and pathological findings. This ensures that patients who do not require intervention are not subjected to unnecessary diagnostic procedures or treatments.
Clinical Implications
Precision Medicine Principles
Adopting a precision medicine approach to coronary care means individualizing diagnostic strategies based on each patient’s unique anatomical and functional characteristics. By integrating advanced diagnostic tools and focusing on comprehensive vascular assessments, clinicians can provide more accurate diagnoses, personalize intervention strategies, and improve overall patient outcomes.
- Individualized Diagnostic Approach: Every patient is different, and coronary flow dynamics will vary from person to person. Tailoring diagnostic assessments to each patient’s specific needs ensures the most effective care.
- Comprehensive Vascular Territory Assessment: A holistic approach that includes a detailed assessment of all coronary territories is critical for identifying the full extent of disease and guiding appropriate treatment decisions.
- Data-Driven Intervention Strategies: Relying on objective data from advanced imaging and flow analyses helps clinicians make evidence-based decisions that maximize treatment effectiveness and patient safety.
Emerging Perspectives
The future of coronary care lies in integrated diagnostic technologies that offer a complete understanding of coronary flow dynamics. Advances in real-time imaging, flow quantification, and artificial intelligence will further enhance the precision of coronary diagnostics, enabling personalized intervention strategies that improve long-term patient outcomes.
As the field of precision cardiology continues to evolve, healthcare professionals must embrace a holistic, technology-driven approach that sees beyond traditional diagnostic boundaries. By integrating advanced imaging, comprehensive flow analysis, and personalized strategies, clinicians can navigate the complexities of coronary artery disease with greater accuracy and precision, ultimately enhancing the quality of care for patients with complex coronary challenges.