Presented by: Tom L. Rosamond, MD, MSc, FAHA, FACC, FASE
Dr. Thomas Rosamond is Board Certified in Cardiovascular Disease. Dr. Rosamond is the Division Chief of Cardiovascular Imaging and Medical Director of Non-Invasive Imaging Services at The University of Kansas Health System. He earned his Postdoctoral Fellowship in Cardiovascular Magnetic Resonance Imaging at Washington University School of Medicine -Barnes Jewish Hospital in St. Louis, Missouri.
Beyond Traditional Diagnosis: Hypertrophic Cardiomyopathy’s Hidden Complexities
Hypertrophic cardiomyopathy (HCM) is one of the most common inherited cardiovascular diseases, yet it remains a diagnostic challenge for many healthcare professionals. This complex disorder, characterized by abnormal thickening of the heart muscle, often presents with subtle, varied symptoms that can be easily missed or misdiagnosed, particularly using traditional diagnostic techniques. In this context, a sophisticated, multi-faceted approach to diagnosis is essential for identifying and managing this condition effectively. This article explores the critical diagnostic considerations and emerging techniques that are advancing the way we understand and detect HCM.
Understanding the Diagnostic Challenge
HCM is a condition that affects both the structural and functional aspects of the heart. While the most well-known clinical feature is hypertrophy of the left ventricle, its presentation can vary significantly. Patients may be asymptomatic or exhibit signs that mimic other cardiovascular or non-cardiovascular diseases, leading to missed or delayed diagnoses. The condition can also present with sudden cardiac death, making early detection and precise diagnosis essential for risk stratification and management.
Given this variability in presentation, healthcare professionals must adopt a more comprehensive approach to diagnosis, incorporating advanced imaging modalities and recognizing the hidden complexities of this condition. In this article, we discuss the key diagnostic considerations and the role of emerging technologies, with a particular focus on how multi-modal imaging strategies can improve outcomes for patients with HCM.
Key Diagnostic Considerations
Comprehensive Imaging Approach
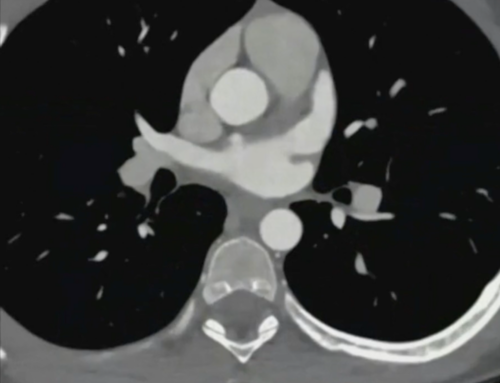
The diagnosis of HCM often involves multiple steps, beginning with a detailed patient history, clinical examination, and electrocardiogram (ECG). However, these standard methods alone are often insufficient for providing a comprehensive assessment of the condition. Imaging plays a central role in confirming a diagnosis, identifying the specific location and extent of myocardial hypertrophy, and evaluating for other complicating factors, such as microvascular dysfunction or ischemia.
Multiple Imaging Modalities Critical for Accurate Diagnosis
While echocardiography has long been the first-line imaging technique for diagnosing HCM, it is not always sufficient on its own. Additional imaging modalities, including cardiac magnetic resonance imaging (MRI), positron emission tomography (PET) CT, and coronary angiography, may be necessary to fully assess the severity of the disease and its impact on heart function. These techniques can provide insights into aspects of the disease that traditional imaging cannot, such as microvascular dysfunction or subclinical ischemia.
Limitations of Single Diagnostic Techniques
Echocardiography, while useful in detecting myocardial hypertrophy and structural abnormalities, often fails to provide the necessary resolution for identifying microvascular dysfunction or accurately assessing perfusion in the myocardium. Similarly, conventional ECG findings may miss early-stage or subclinical cases of HCM, particularly in patients without overt symptoms. Therefore, relying on a single diagnostic tool can lead to misdiagnosis or underdiagnosis of HCM, emphasizing the need for integrative diagnostic strategies.
Importance of Integrative Diagnostic Strategies
An integrative diagnostic strategy combines multiple imaging modalities and diagnostic tests to provide a more accurate and complete picture of the patient’s condition. By using a combination of techniques—each providing unique insights—clinicians can better identify and evaluate all aspects of HCM, including its structural and functional components.
Advanced Detection Techniques
Diagnostic Red Flags
There are several key diagnostic indicators that healthcare professionals should look for when suspecting HCM. Early identification of these signs can be crucial in preventing adverse outcomes, particularly in high-risk patients.
Electrocardiographic Indicators
- Classic T-Wave Inversions: One of the hallmark ECG findings in HCM is T-wave inversions, often seen in the precordial leads. While this can be indicative of several cardiac conditions, when observed in conjunction with other diagnostic findings, it raises suspicion for HCM.
- Apical Hypertrophy Patterns: In some cases, especially in older patients, HCM may present with apical hypertrophy, a form of thickening that occurs in the tip of the left ventricle. This may not always be evident on routine ECG, making advanced imaging crucial for confirmation.
Echocardiographic Findings
- Excessive Myocardial Hypertrophy: Echocardiography typically reveals excessive hypertrophy of the left ventricle, particularly in the interventricular septum. The extent of this hypertrophy can guide risk assessment and determine the need for further imaging or interventions.
- Subepicardial Layer Impingement: Another important echocardiographic finding in HCM is subepicardial layer impingement, where the thickened myocardium compromises blood flow to the outer layers of the heart muscle.
- Cavity Deformations: In more advanced cases, the left ventricle may exhibit deformations, such as abnormal chamber size or shape, that affect the heart’s ability to pump blood efficiently.
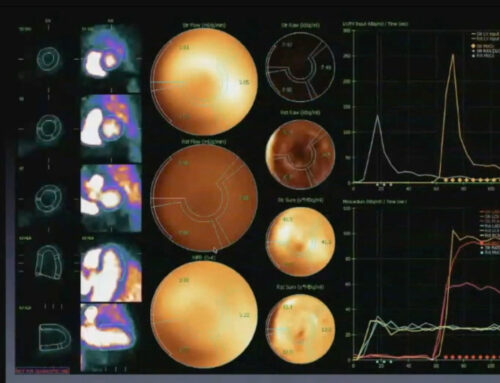
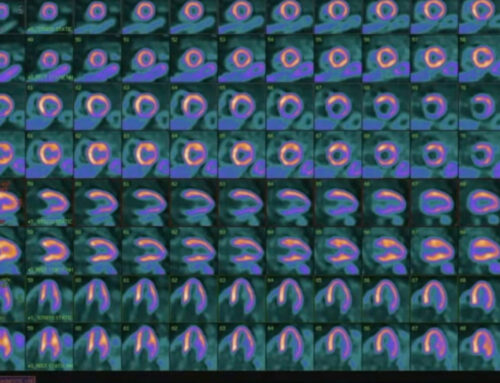
PET CT Revelations
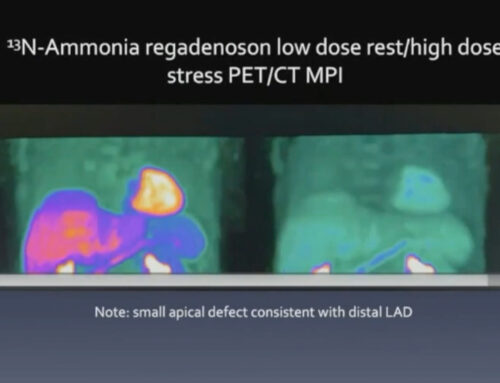
PET CT imaging, particularly when combined with nitrogen ammonia imaging, has emerged as a powerful tool for detecting and evaluating HCM.
- Splenic Switch-Off Sign: One of the critical stress validation markers identified by PET CT is the splenic switch-off sign, which indicates reduced myocardial blood flow during periods of stress. This sign can be a critical indicator of microvascular dysfunction in HCM patients, providing early evidence of ischemia or other perfusion abnormalities.
- Detailed Visualization of Microvascular Dysfunction: PET CT offers a unique advantage by allowing clinicians to visualize microvascular dysfunction, a key feature of HCM that cannot be detected through traditional imaging. Microvascular dysfunction is often present in HCM patients even in the absence of overt coronary artery disease, and its detection can guide more precise treatment strategies.
- Differentiation Between Structural and Functional Abnormalities: PET CT can also help differentiate between structural abnormalities (such as myocardial hypertrophy) and functional abnormalities (such as ischemia), allowing for more tailored management strategies.
Microvascular Dysfunction: A Crucial Insight
A hallmark of HCM that has garnered increased attention in recent years is microvascular dysfunction. This phenomenon refers to impaired blood flow in the small coronary vessels, which can lead to myocardial ischemia even in the absence of obstructive coronary artery disease.
Universal Microvascular Disease Characteristics
Microvascular dysfunction in HCM is characterized by:
- Consistent Flow Patterns Across Epicardial Coronary Vessels: Unlike coronary artery disease, where blood flow is typically restricted in the epicardial arteries, microvascular disease in HCM affects the small vessels within the heart muscle, disrupting blood flow across all layers of the myocardium.
- Low Quantitative Measurements: PET CT and other imaging modalities can detect low quantitative measurements of myocardial perfusion, which may not be evident on other forms of imaging, such as coronary angiography.
- Common Across HCM Subtypes: Microvascular dysfunction is seen across a range of HCM subtypes, regardless of the genetic mutation responsible for the disease, making it a universal characteristic of the condition.
Clinical Implications
Diagnostic Recommendations
To improve diagnostic accuracy and patient outcomes, healthcare professionals should:
- Utilize Multi-Modal Imaging Techniques: Combining modalities such as echocardiography, MRI, PET CT, and coronary angiography allows for a more comprehensive and accurate diagnosis of HCM.
- Look Beyond Traditional Coronary Assessments: Since microvascular dysfunction is a central feature of HCM, clinicians must incorporate advanced imaging techniques that can identify these abnormalities, even in the absence of coronary artery disease.
- Recognize Subtle Microvascular Changes: Identifying early signs of microvascular dysfunction can be critical in guiding treatment decisions, particularly in patients with mild or subclinical forms of HCM.
- Understand Ischemic Patterns in Hypertrophic Conditions: Recognizing the ischemic patterns that arise from hypertrophy and microvascular dysfunction can lead to better risk stratification and more personalized management plans.
Emerging Perspectives
The future of HCM diagnosis lies in harnessing the power of advanced imaging technologies and comprehensive metabolic and functional assessments. These precision diagnostic approaches will enable healthcare professionals to diagnose HCM earlier, assess disease progression more effectively, and tailor treatments to individual patients, ultimately improving long-term outcomes.
Hypertrophic cardiomyopathy represents a complex and often elusive condition that demands a sophisticated, layered diagnostic strategy. As advancements in imaging technologies continue to evolve, healthcare professionals have the tools to look beyond traditional diagnostic methods, offering a more complete understanding of the disease and its progression. By integrating multi-modal imaging, recognizing the hidden complexities of microvascular dysfunction, and adopting a precision approach to diagnosis, clinicians can provide more accurate diagnoses and personalized treatments, ultimately improving outcomes for patients with HCM.